MENOPAUSE AND HORMONE REPLACEMENT THERAPY IS A HOT TOPIC OF CONVERSATION LATELY.
What do we know about hormone therapy? Who’s it good for? What are the risks and benefits? One thing we know for sure, there is no one-size-fits-all.
In this guide we’re going to talk about the Women’s Health Initiative study involving over 26,000 women taking hormone therapy. This study provided valuable insight about the risks and benefits to hormone therapy, and who should take it, and at what stage and age. We will also provide definitions of the different types of hormone therapy, discuss bioidentical hormones and compound-formulations.
If you’re wondering, “Is it right for me?” The answer, as with most complicated questions, is, “It depends.” This guide is designed to provide information and education about hormone therapy that coupled with your personal and lifestyle values and beliefs, can help you make an informed decision. And that decision needs to be made in consultation with your healthcare provider who can assess the health risks present based on your medical history.
WHAT IS MENOPAUSE
Menopause is defined as 12 consecutive months from your last menstruation. It is often accompanied by a range of physical and psychological symptoms, including hot flashes, night sweats, vaginal dryness, mood changes, and sleep disturbances. Hormone therapy is a common treatment option that has been used to manage these symptoms for many years. Hormone therapy involves the use of estrogen or combined estrogen and progestin hormones to replace the natural hormones that are no longer produced by the ovaries after menopause.
HORMONE THERAPY, BIOIDENTICAL HORMONE THERAPY AND CUSTOM-COMPOUNDED HORMONES
WHAT IS HORMONE THERAPY (HT)?
a.k.a Hormone Replacement Therapy (HRT) and Menopausal Hormone Therapy (MHT)
Hormone therapy is used to relieve some menopausal symptoms. According to The North American Menopause Society (NAMS), “Hormone therapies are the prescription drugs used most often to treat hot flashes and genitourinary syndrome of menopause (GMS), which includes vaginal dryness after menopause.”
WHAT IS BIOIDENTICAL HORMONE THERAPY (BHT)?
According to The Society of Obstetricians and Gynaecologists of Canada (SOGC),
“The term “bioidentical hormone therapy” is often used to describe a medication containing estrogen, progesterone, or other hormones that are chemically exact duplicates of hormones produced by women, primarily in the ovaries. Many of these body-identical hormones are commercially available in several well-tested, Health Canada approved, brand-name prescription drugs.” These synthetic hormones come from plant sources that have been chemically modified to be identical to human hormones – hence described as “bioidentical”.
BHT originated as a marketing term for custom-compounded hormones, but can also mean hormones that take the same chemical and molecular structure as the ones we create in our bodies. There are many FDA approved products that fall under this classification. And then there are the custom compounded hormones.
WHAT ABOUT CUSTOM-COMPOUNDED HORMONES?
Custom-compounded hormones are custom mixed prescriptions with non-standard doses as an individualized solution. They are not regulated by the FDA meaning they vary in strength and purity.
What are the trusted resources saying? Guidelines from the American College of Obstetricians and Gynaecologists say conventional HT is preferred over custom compounded formulas. The American Association of Clinical Endocrinologists recommend against it.
Echoing the sentiment is SOGC who supports the 2017 NAMS statement on Bioidentical Hormone Therapy.
“Compounded bioidentical HT presents safety concerns such as minimal government regulation and monitoring, overdosing or under-dosing, presence of impurities or lack of sterility, lack of scientific efficacy and safety data, and lack of a label outlining risks.”
The NAMS positioning statement also states:
“Situations in which compounded bioidentical hormones could be considered include allergies to ingredients in a govern-approved formulation or dosages not available in government-approved products.”
While there is no scientific support for any advantages of these compounds over approved preparations, they have gained popularity and many women are taking this approach. Women should be aware of the risk involved with taking non-standardized medication and consult with their healthcare provider.
Compounded hormone therapy allows for customized dosing. With compounding there is the ability to create lower doses, meaning women who are hormone sensitive can still explore the option of hormone therapy. Compounded versions are also an option for women who have allergies or sensitivities to fillers in the government approved products. It allows the approach to be more individualized when needed. It is important to use a reliable and reputable pharmacy.
WHAT ARE THE TYPES OF HORMONE THERAPY?
As defined by the NAMS, there are two basic types of hormone therapy and two general ways to take hormone therapy:
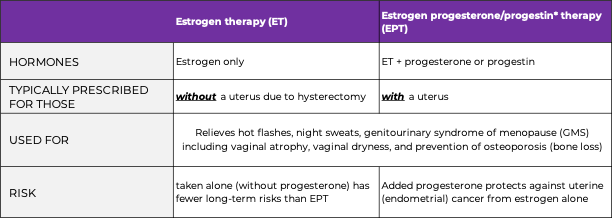
*progestin is a synthetic form of progesterone
There are two general ways to take hormone therapy:
- Systemic products. They circulate through the bloodstream to all parts of the body and typically used for night sweats, hot flashes, vaginal symptoms, and osteoporosis. They can come in many formats including pill, patch, gel, emulsion, spray or injection.
- Local (non-systemic) products. These affect only a specific or localized area of the body and can be used for vaginal symptoms. They come in the form of cream, ring or tablet. Vaginal estrogen therapy (administered in the vagina) for vaginal symptoms after menopause can moisturize and rebuild tissue with little going into blood circulation, making risks much lower, and more effective for vaginal symptoms than systemic.
As with all medications, there are a variety of side effects to consider include bleeding or irregular spotting, weight gain (fluid retention), headaches/migraines, breast tenderness, increased breast density or dark skin spots.
With the information learned from the Woman’s Health Initiative Study, a much shorter duration (3-5 years) and lower doses of HT are being prescribed. The NAMS Position Statement recommends that women use the lowest effective dose of HRT for the shortest duration necessary to achieve treatment goals, and that they be monitored regularly by their healthcare provider for potential side effects or risks.
Always consult with your healthcare provider to determine if you are a candidate for hormone therapy.
THE WOMEN’S HEALTH INITIATIVE STUDY (WHI)
Most of what we know today about hormone therapy stems from The WHI Clinical Trial. The Women’s Health Initiative studied the long-term effects of hormone therapy in healthy postmenopausal women aged 50 to 79 years old from 1993 to 1998. 16,608 women with uteri received combinations of estrogen and progesterone, or placebo; and 10,739 women without uteri received estrogen or placebo.
The focus of the study was to define risks and benefits of strategies that could reduce heart disease, breast and colorectal cancer and fractures in post-menopausal women. It was not designed to test the short-term effects of hormone therapy.
The study ended early in 2002 due to findings of increased breast cancer, heart disease, stroke, blood clots and dementia for women receiving estrogen plus progestin compared to those who took placebo. For those who had a prior hysterectomy and taking estrogen only therapy, there was an increased risk for stroke and blood clots. These risks are potentially increased from the hormone formulation, higher dosing and initiation of hormone prescriptions too late after menopause.
The data from this trial has been the basis of treatment and dosage recommendations, and in particular for women under the age of 60, and less than 10 years from their last period. They found the treatment was most safe and effective on newly menopausal women — that is women who take estrogen soon after reaching menopause.
WHAT ARE THE BENEFITS AND RISKS OF HORMONE THERAPY?
There have been hundreds of clinical studies providing evidence that systemic hormone therapy (ET or EPT) helps relieve symptoms. Addressing these root cause symptoms can provide benefits of improved sleep, sex and overall quality of life.
The risks associated with HT is primarily focused on women over 60 years old, or when systemic ET or EPT is taken long-term (5+ years). It is often recommended to start hormone therapy in the 1 to 3 years leading up to menopause to address symptoms such as hot flashes and soon after becoming menopausal, lowering the risk than starting later.
Let’s look at both sides.
BENEFITS:
Symptom relief: Hormone therapy is the most effective treatment option for relieving hot flashes, night sweats, mood or vaginal atrophy and dryness.
Bone health: HT has been shown to reduce the risk of osteoporosis and fractures in postmenopausal women. Estrogen therapy helps to maintain bone density.
Brain health: Using hormone therapy in early menopause for women at risk of Alzheimer’s has benefits for prevention of Alzheimer’s
Quality of life: overall quality of life for women experiencing menopausal symptoms including improved sleep, mood, and sexual function may be improved with the use of HT.
RISKS:
Breast cancer: According to the NAMS 2022 Position Statement on Hormone Therapy the risk for breast cancer is low, and estimates less than 1 additional case per 1,000 women per year of hormone therapy use or 3 additional cases per 1,000 women per year when used for 5 years of EPT. It’s important to know that some types of HT are associated with increased breast density which makes cancer screening more difficult.
Endometrial cancer: Women who have a uterus and use estrogen therapy alone (meaning, without progestin) are at an increased risk of developing endometrial cancer. Addition of progestogen to estrogen therapy reduces this risk.
Coronary heart disease: HT initiated after the age of 60 and more than 10 or 20 years from menopause onset have a higher risk of coronary heart disease.
Venous thromboembolism: Hormone therapy has been associated with an increased risk of blood clots in the veins.
Stroke: HT has been associated with an increased risk of blood clots and stroke in some women.
Gallbladder disease: The use of ET and EPT has been associated with an increased risk of gallbladder disease (gallbladder/gallstone problems).
Brain health: there is an increased risk of dementia if HT is started after 65 years of age, and taking it for more than 5 years.
Additional risks: increased risk of ovarian cancer with long-term use, and increased risk of cardiovascular events in older women or those with pre-existing cardiovascular disease. As well the increase in urinary incontinence.
You can start to see the complexity of a risk/benefit analysis when determining what is right for you. What the experts want us to know is they support hormone therapy for treating moderate to severe symptoms, and that its health benefits outweigh the risks. We need to know this information to inform our choices taking into account our personal opinion of taking hormones versus trying natural options, or other prescriptions.
RISKS OF HORMONE THERAPY AFTER CANCER
The NAMS 2022 Position Statement on Hormone Therapy provides key points about HT after certain cancers, in particular breast, endometrial, ovarian, colorectal and lung. In general, hormone therapy is not recommended, however there are some very specific examples where it may be considered in consultation with one’s doctor and oncologist.
The Canadian Cancer Society recommends “women with a history of breast cancer may be advised not to take HRT.” The main concern is the estrogen could cause the breast cancer to return. The risk is not fully understood as there are different studies indicating different things about the effects of HT on women who have or have had breast cancer.
The Canadian Cancer Society goes on to say “HRT may be an option for women at a higher risk for breast cancer.” It is typically not advised, but it might be with the right counselling and follow-up for severe vasomotor symptoms that are not responding to non-hormonal options.
ALTERNATIVES TO HORMONE THERAPY
Many women are interested in options other than hormone therapy to treat menopause symptoms Alternatives include:
- Over-the-counter vaginal moisturizers and lubricants
- Non-hormonal medications, including:
- Antidepressants—to relieve hot flashes
- Selective estrogen modulators (SERMs)—to relieve hot flashes or pain during sex
- A daily vaginal insert called dehydroepiandrosterone (DHEA)—to relieve pain during sex
- A seizure medication called gabapentin and a blood pressure medication called clonidine—to reduce hot flashes and ease sleep problems
- Plant and herbal supplements, including some soy products
You can read our previous blog post which goes into more detail about natural, non-hormone remedies for hot flashes
On May 12, 2023, the FDA approved a drug that relieves hot flashes. Veovah (fezolinetant) is non-hormonal and requires blood tests to look for liver damage before and while taking the drug for the first 9 months. This is in connection to its most severe possible side effect being livery injury known as elevated hepatic transaminase.
While this drug is a new (non-hormonal) tool in the box for treating hot flashes, most medical professionals still recommend HT as a first choice if it is right for you. This drug will be available in the US three weeks from its approval, and it is worth noting long-term studies have yet to be conducted for this drug.
SO HOW DO I DECIDE?
It’s good to remember each of us is unique, and we must weigh the pros and cons of our healthcare choices independent of our friends and family. Symptoms, age, health history and family history differ along with our beliefs and values.
Hormone therapy has been scientifically proven to effectively help relieve menopausal symptoms, and has the added benefit of heart, brain, bone and vaginal health. However, hormone therapy is not for everyone, whether by personal choice, or due to previous health conditions that make it a no-go. There are non-hormonal options such as dietary changes, exercise and weight management, meditation, and natural therapies that can bring relief from mild symptoms.
The best way to decide is to be informed. Educate yourself and speak to your healthcare professional who is well-educated about menopause and hormone therapies. Come armed with questions, voice your concerns and together weigh the benefits and risks against the expected duration of your treatment.
And remember, our bodies keep changing over time, so it is important to re-evaluate and make adjustments with your practitioner regularly. Speak candidly. Only you and your healthcare provider can determine what is right.
If you are looking for a healthcare provider with advanced training in menopause, book a free mini consult with us to start the discussion.
WRITTEN BY: AlterEgo Health
EDITED BY: Dr. Christine Kadykalo ND, MSCP
DISCLAIMER: The health, fitness and nutritional information and content provided is for general educational and informational purposes only and is not professional medical advice, diagnosis, treatment or care, nor is it intended to be a substitute therefor. If you have any concerns or questions about your health, always seek the advice of a doctor or other qualified health care professional. Do not disregard, avoid or delay in seeking medical advice or treatment from your health care professional because of something you have read here. Please refer to our Terms of Use for further information on the terms and conditions that govern your use of the website and any material provided therein, including this article.
Education, Feature
Education, Feature
NOT FEELING IT? IT DOESN'T NECESSARILY MEAN YOU'VE LOST INTEREST IN SEX OR YOUR PARTNER. CAN'T GET ENOUGH? THAT COULD BE FREEDOM CALLING KNOWING YOU CAN'T GET PREGNANT. HOWEVER YOU ...
NOT FEELING IT? IT DOESN'T NECESSARILY MEAN YOU'VE LOST INTEREST ...
Education, Feature
Education, Feature
MENOPAUSE AND HORMONE REPLACEMENT THERAPY IS A HOT TOPIC OF CONVERSATION LATELY. What do we know about hormone therapy? Who’s it good for? What are the risks and benefits? ...
MENOPAUSE AND HORMONE REPLACEMENT THERAPY IS A HOT TOPIC ...
Education, Symptoms
Education, Symptoms
ANYONE ELSE ON FIRE?! Hot flashes seem to come out of nowhere, and are very good at choosing inopportune times to show up. Uninvited. Just ask Drew Barrymore when she ...
ANYONE ELSE ON FIRE?! Hot flashes seem to come out ...
MENOPAUSE AND HORMONE REPLACEMENT THERAPY IS A HOT TOPIC OF CONVERSATION LATELY.
What do we know about hormone therapy? Who’s it good for? What are the risks and benefits? One thing we know for sure, there is no one-size-fits-all.
In this guide we’re going to talk about the Women’s Health Initiative study involving over 26,000 women taking hormone therapy. This study provided valuable insight about the risks and benefits to hormone therapy, and who should take it, and at what stage and age. We will also provide definitions of the different types of hormone therapy, discuss bioidentical hormones and compound-formulations.
If you’re wondering, “Is it right for me?” The answer, as with most complicated questions, is, “It depends.” This guide is designed to provide information and education about hormone therapy that coupled with your personal and lifestyle values and beliefs, can help you make an informed decision. And that decision needs to be made in consultation with your healthcare provider who can assess the health risks present based on your medical history.
WHAT IS MENOPAUSE
Menopause is defined as 12 consecutive months from your last menstruation. It is often accompanied by a range of physical and psychological symptoms, including hot flashes, night sweats, vaginal dryness, mood changes, and sleep disturbances. Hormone therapy is a common treatment option that has been used to manage these symptoms for many years. Hormone therapy involves the use of estrogen or combined estrogen and progestin hormones to replace the natural hormones that are no longer produced by the ovaries after menopause.
HORMONE THERAPY, BIOIDENTICAL HORMONE THERAPY AND CUSTOM-COMPOUNDED HORMONES
WHAT IS HORMONE THERAPY (HT)?
a.k.a Hormone Replacement Therapy (HRT) and Menopausal Hormone Therapy (MHT)
Hormone therapy is used to relieve some menopausal symptoms. According to The North American Menopause Society (NAMS), “Hormone therapies are the prescription drugs used most often to treat hot flashes and genitourinary syndrome of menopause (GMS), which includes vaginal dryness after menopause.”
WHAT IS BIOIDENTICAL HORMONE THERAPY (BHT)?
According to The Society of Obstetricians and Gynaecologists of Canada (SOGC),
“The term “bioidentical hormone therapy” is often used to describe a medication containing estrogen, progesterone, or other hormones that are chemically exact duplicates of hormones produced by women, primarily in the ovaries. Many of these body-identical hormones are commercially available in several well-tested, Health Canada approved, brand-name prescription drugs.” These synthetic hormones come from plant sources that have been chemically modified to be identical to human hormones – hence described as “bioidentical”.
BHT originated as a marketing term for custom-compounded hormones, but can also mean hormones that take the same chemical and molecular structure as the ones we create in our bodies. There are many FDA approved products that fall under this classification. And then there are the custom compounded hormones.
WHAT ABOUT CUSTOM-COMPOUNDED HORMONES?
Custom-compounded hormones are custom mixed prescriptions with non-standard doses as an individualized solution. They are not regulated by the FDA meaning they vary in strength and purity.
What are the trusted resources saying? Guidelines from the American College of Obstetricians and Gynaecologists say conventional HT is preferred over custom compounded formulas. The American Association of Clinical Endocrinologists recommend against it.
Echoing the sentiment is SOGC who supports the 2017 NAMS statement on Bioidentical Hormone Therapy.
“Compounded bioidentical HT presents safety concerns such as minimal government regulation and monitoring, overdosing or under-dosing, presence of impurities or lack of sterility, lack of scientific efficacy and safety data, and lack of a label outlining risks.”
The NAMS positioning statement also states:
“Situations in which compounded bioidentical hormones could be considered include allergies to ingredients in a govern-approved formulation or dosages not available in government-approved products.”
While there is no scientific support for any advantages of these compounds over approved preparations, they have gained popularity and many women are taking this approach. Women should be aware of the risk involved with taking non-standardized medication and consult with their healthcare provider.
Compounded hormone therapy allows for customized dosing. With compounding there is the ability to create lower doses, meaning women who are hormone sensitive can still explore the option of hormone therapy. Compounded versions are also an option for women who have allergies or sensitivities to fillers in the government approved products. It allows the approach to be more individualized when needed. It is important to use a reliable and reputable pharmacy.
WHAT ARE THE TYPES OF HORMONE THERAPY?
As defined by the NAMS, there are two basic types of hormone therapy and two general ways to take hormone therapy:
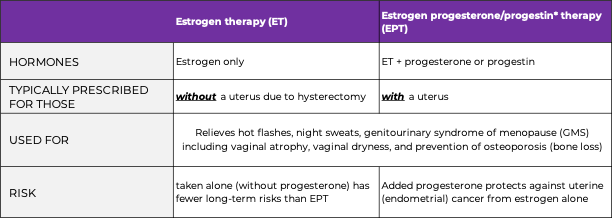
*progestin is a synthetic form of progesterone
There are two general ways to take hormone therapy:
- Systemic products. They circulate through the bloodstream to all parts of the body and typically used for night sweats, hot flashes, vaginal symptoms, and osteoporosis. They can come in many formats including pill, patch, gel, emulsion, spray or injection.
- Local (non-systemic) products. These affect only a specific or localized area of the body and can be used for vaginal symptoms. They come in the form of cream, ring or tablet. Vaginal estrogen therapy (administered in the vagina) for vaginal symptoms after menopause can moisturize and rebuild tissue with little going into blood circulation, making risks much lower, and more effective for vaginal symptoms than systemic.
As with all medications, there are a variety of side effects to consider include bleeding or irregular spotting, weight gain (fluid retention), headaches/migraines, breast tenderness, increased breast density or dark skin spots.
With the information learned from the Woman’s Health Initiative Study, a much shorter duration (3-5 years) and lower doses of HT are being prescribed. The NAMS Position Statement recommends that women use the lowest effective dose of HRT for the shortest duration necessary to achieve treatment goals, and that they be monitored regularly by their healthcare provider for potential side effects or risks.
Always consult with your healthcare provider to determine if you are a candidate for hormone therapy.
THE WOMEN’S HEALTH INITIATIVE STUDY (WHI)
Most of what we know today about hormone therapy stems from The WHI Clinical Trial. The Women’s Health Initiative studied the long-term effects of hormone therapy in healthy postmenopausal women aged 50 to 79 years old from 1993 to 1998. 16,608 women with uteri received combinations of estrogen and progesterone, or placebo; and 10,739 women without uteri received estrogen or placebo.
The focus of the study was to define risks and benefits of strategies that could reduce heart disease, breast and colorectal cancer and fractures in post-menopausal women. It was not designed to test the short-term effects of hormone therapy.
The study ended early in 2002 due to findings of increased breast cancer, heart disease, stroke, blood clots and dementia for women receiving estrogen plus progestin compared to those who took placebo. For those who had a prior hysterectomy and taking estrogen only therapy, there was an increased risk for stroke and blood clots. These risks are potentially increased from the hormone formulation, higher dosing and initiation of hormone prescriptions too late after menopause.
The data from this trial has been the basis of treatment and dosage recommendations, and in particular for women under the age of 60, and less than 10 years from their last period. They found the treatment was most safe and effective on newly menopausal women — that is women who take estrogen soon after reaching menopause.
WHAT ARE THE BENEFITS AND RISKS OF HORMONE THERAPY?
There have been hundreds of clinical studies providing evidence that systemic hormone therapy (ET or EPT) helps relieve symptoms. Addressing these root cause symptoms can provide benefits of improved sleep, sex and overall quality of life.
The risks associated with HT is primarily focused on women over 60 years old, or when systemic ET or EPT is taken long-term (5+ years). It is often recommended to start hormone therapy in the 1 to 3 years leading up to menopause to address symptoms such as hot flashes and soon after becoming menopausal, lowering the risk than starting later.
Let’s look at both sides.
BENEFITS:
Symptom relief: Hormone therapy is the most effective treatment option for relieving hot flashes, night sweats, mood or vaginal atrophy and dryness.
Bone health: HT has been shown to reduce the risk of osteoporosis and fractures in postmenopausal women. Estrogen therapy helps to maintain bone density.
Brain health: Using hormone therapy in early menopause for women at risk of Alzheimer’s has benefits for prevention of Alzheimer’s
Quality of life: overall quality of life for women experiencing menopausal symptoms including improved sleep, mood, and sexual function may be improved with the use of HT.
RISKS:
Breast cancer: According to the NAMS 2022 Position Statement on Hormone Therapy the risk for breast cancer is low, and estimates less than 1 additional case per 1,000 women per year of hormone therapy use or 3 additional cases per 1,000 women per year when used for 5 years of EPT. It’s important to know that some types of HT are associated with increased breast density which makes cancer screening more difficult.
Endometrial cancer: Women who have a uterus and use estrogen therapy alone (meaning, without progestin) are at an increased risk of developing endometrial cancer. Addition of progestogen to estrogen therapy reduces this risk.
Coronary heart disease: HT initiated after the age of 60 and more than 10 or 20 years from menopause onset have a higher risk of coronary heart disease.
Venous thromboembolism: Hormone therapy has been associated with an increased risk of blood clots in the veins.
Stroke: HT has been associated with an increased risk of blood clots and stroke in some women.
Gallbladder disease: The use of ET and EPT has been associated with an increased risk of gallbladder disease (gallbladder/gallstone problems).
Brain health: there is an increased risk of dementia if HT is started after 65 years of age, and taking it for more than 5 years.
Additional risks: increased risk of ovarian cancer with long-term use, and increased risk of cardiovascular events in older women or those with pre-existing cardiovascular disease. As well the increase in urinary incontinence.
You can start to see the complexity of a risk/benefit analysis when determining what is right for you. What the experts want us to know is they support hormone therapy for treating moderate to severe symptoms, and that its health benefits outweigh the risks. We need to know this information to inform our choices taking into account our personal opinion of taking hormones versus trying natural options, or other prescriptions.
RISKS OF HORMONE THERAPY AFTER CANCER
The NAMS 2022 Position Statement on Hormone Therapy provides key points about HT after certain cancers, in particular breast, endometrial, ovarian, colorectal and lung. In general, hormone therapy is not recommended, however there are some very specific examples where it may be considered in consultation with one’s doctor and oncologist.
The Canadian Cancer Society recommends “women with a history of breast cancer may be advised not to take HRT.” The main concern is the estrogen could cause the breast cancer to return. The risk is not fully understood as there are different studies indicating different things about the effects of HT on women who have or have had breast cancer.
The Canadian Cancer Society goes on to say “HRT may be an option for women at a higher risk for breast cancer.” It is typically not advised, but it might be with the right counselling and follow-up for severe vasomotor symptoms that are not responding to non-hormonal options.
ALTERNATIVES TO HORMONE THERAPY
Many women are interested in options other than hormone therapy to treat menopause symptoms Alternatives include:
- Over-the-counter vaginal moisturizers and lubricants
- Non-hormonal medications, including:
- Antidepressants—to relieve hot flashes
- Selective estrogen modulators (SERMs)—to relieve hot flashes or pain during sex
- A daily vaginal insert called dehydroepiandrosterone (DHEA)—to relieve pain during sex
- A seizure medication called gabapentin and a blood pressure medication called clonidine—to reduce hot flashes and ease sleep problems
- Plant and herbal supplements, including some soy products
You can read our previous blog post which goes into more detail about natural, non-hormone remedies for hot flashes
On May 12, 2023, the FDA approved a drug that relieves hot flashes. Veovah (fezolinetant) is non-hormonal and requires blood tests to look for liver damage before and while taking the drug for the first 9 months. This is in connection to its most severe possible side effect being livery injury known as elevated hepatic transaminase.
While this drug is a new (non-hormonal) tool in the box for treating hot flashes, most medical professionals still recommend HT as a first choice if it is right for you. This drug will be available in the US three weeks from its approval, and it is worth noting long-term studies have yet to be conducted for this drug.
SO HOW DO I DECIDE?
It’s good to remember each of us is unique, and we must weigh the pros and cons of our healthcare choices independent of our friends and family. Symptoms, age, health history and family history differ along with our beliefs and values.
Hormone therapy has been scientifically proven to effectively help relieve menopausal symptoms, and has the added benefit of heart, brain, bone and vaginal health. However, hormone therapy is not for everyone, whether by personal choice, or due to previous health conditions that make it a no-go. There are non-hormonal options such as dietary changes, exercise and weight management, meditation, and natural therapies that can bring relief from mild symptoms.
The best way to decide is to be informed. Educate yourself and speak to your healthcare professional who is well-educated about menopause and hormone therapies. Come armed with questions, voice your concerns and together weigh the benefits and risks against the expected duration of your treatment.
And remember, our bodies keep changing over time, so it is important to re-evaluate and make adjustments with your practitioner regularly. Speak candidly. Only you and your healthcare provider can determine what is right.
If you are looking for a healthcare provider with advanced training in menopause, book a free mini consult with us to start the discussion.
WRITTEN BY: AlterEgo Health
EDITED BY: Dr. Christine Kadykalo ND, MSCP
DISCLAIMER: The health, fitness and nutritional information and content provided is for general educational and informational purposes only and is not professional medical advice, diagnosis, treatment or care, nor is it intended to be a substitute therefor. If you have any concerns or questions about your health, always seek the advice of a doctor or other qualified health care professional. Do not disregard, avoid or delay in seeking medical advice or treatment from your health care professional because of something you have read here. Please refer to our Terms of Use for further information on the terms and conditions that govern your use of the website and any material provided therein, including this article.
Education, Feature
Education, Feature
NOT FEELING IT? IT DOESN'T NECESSARILY MEAN YOU'VE LOST INTEREST IN SEX OR YOUR PARTNER. CAN'T GET ENOUGH? THAT COULD BE FREEDOM CALLING KNOWING YOU CAN'T GET PREGNANT. HOWEVER YOU ...
NOT FEELING IT? IT DOESN'T NECESSARILY MEAN YOU'VE LOST INTEREST ...
Education, Feature
Education, Feature
MENOPAUSE AND HORMONE REPLACEMENT THERAPY IS A HOT TOPIC OF CONVERSATION LATELY. What do we know about hormone therapy? Who’s it good for? What are the risks and benefits? ...
MENOPAUSE AND HORMONE REPLACEMENT THERAPY IS A HOT TOPIC ...
Education, Symptoms
Education, Symptoms
ANYONE ELSE ON FIRE?! Hot flashes seem to come out of nowhere, and are very good at choosing inopportune times to show up. Uninvited. Just ask Drew Barrymore when she ...
ANYONE ELSE ON FIRE?! Hot flashes seem to come out ...
Education, Symptoms
Education, Symptoms
"MY PERIOD USED TO BE LIKE CLOCKWORK. NOW IT'S MORE LIKE A GAME OF CHANCE." Unknown One of the firsts signs I was in or entering perimenopause was when my ...
"MY PERIOD USED TO BE LIKE CLOCKWORK. NOW IT'S MORE ...